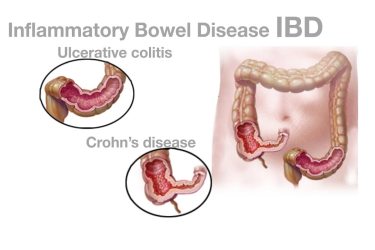
Inflammatory bowel disease (IBD) is a term that describes disorders involving long-standing (chronic) inflammation of tissues in your digestive tract. Types of IBD include:
![]() Ulcerative colitis. This condition involves inflammation and sores (ulcers) along the lining of your large intestine (colon) and rectum.
Ulcerative colitis. This condition involves inflammation and sores (ulcers) along the lining of your large intestine (colon) and rectum.
![]() Crohn's disease. This type of IBD is characterized by inflammation of the lining of your digestive tract, which often can involve the deeper layers of the digestive tract. Crohn's disease most commonly affects the small intestine. However, it can also affect the large intestine and sometimes the upper gastrointestinal tract.
Crohn's disease. This type of IBD is characterized by inflammation of the lining of your digestive tract, which often can involve the deeper layers of the digestive tract. Crohn's disease most commonly affects the small intestine. However, it can also affect the large intestine and sometimes the upper gastrointestinal tract.
Both ulcerative colitis and Crohn's disease usually are characterized by diarrhea, rectal bleeding, abdominal pain, fatigue and weight loss.
For some people, IBD is only a mild illness. For others, it's a debilitating condition that can lead to life-threatening complications.
Inflammatory bowel disease symptoms vary, depending on the severity of inflammation and where it occurs. Symptoms may range from mild to severe. You are likely to have periods of active illness followed by periods of remission.
Signs and symptoms that are common to both Crohn's disease and ulcerative colitis include:
![]() Diarrhea
Diarrhea
![]() Fatigue
Fatigue
![]() Abdominal pain and cramping
Abdominal pain and cramping
![]() Blood in your stool
Blood in your stool
![]() Reduced appetite
Reduced appetite
![]() Unintended weight loss
Unintended weight loss

To help confirm a diagnosis of IBD, you will need a combination of tests and procedures:
![]() Tests for anemia or infection - Your provider may suggest blood tests to check for anemia — a condition in which there aren't enough red blood cells to carry adequate oxygen to your tissues — or to check for signs of infection from bacteria or viruses.
Tests for anemia or infection - Your provider may suggest blood tests to check for anemia — a condition in which there aren't enough red blood cells to carry adequate oxygen to your tissues — or to check for signs of infection from bacteria or viruses.
![]() Stool studies - You may need to provide a stool sample so that your provider can test for hidden (occult) blood or organisms, such as parasites, in your stool.
Stool studies - You may need to provide a stool sample so that your provider can test for hidden (occult) blood or organisms, such as parasites, in your stool.
![]() Colonoscopy - This exam allows your provider to view your entire colon using a thin, flexible, lighted tube with a camera at the end. During the procedure, small samples of tissue (biopsy) may be taken for laboratory analysis. A biopsy is the way to make the diagnosis of IBD versus other forms of inflammation.
Colonoscopy - This exam allows your provider to view your entire colon using a thin, flexible, lighted tube with a camera at the end. During the procedure, small samples of tissue (biopsy) may be taken for laboratory analysis. A biopsy is the way to make the diagnosis of IBD versus other forms of inflammation.
![]() Flexible sigmoidoscopy - Your provider uses a slender, flexible, lighted tube to examine the rectum and sigmoid, the last portion of your colon. If your colon is severely inflamed, your provider may perform this test instead of a full colonoscopy.
Flexible sigmoidoscopy - Your provider uses a slender, flexible, lighted tube to examine the rectum and sigmoid, the last portion of your colon. If your colon is severely inflamed, your provider may perform this test instead of a full colonoscopy.
![]() Upper endoscopy - In this procedure, your provider uses a slender, flexible, lighted tube to examine the esophagus, stomach and first part of the small intestine (duodenum). While it is rare for these areas to be involved with Crohn's disease, this test may be recommended if you are having nausea and vomiting, difficulty eating, or upper abdominal pain.
Upper endoscopy - In this procedure, your provider uses a slender, flexible, lighted tube to examine the esophagus, stomach and first part of the small intestine (duodenum). While it is rare for these areas to be involved with Crohn's disease, this test may be recommended if you are having nausea and vomiting, difficulty eating, or upper abdominal pain.
![]() Capsule endoscopy - This test is sometimes used to help diagnose Crohn's disease involving your small intestine. You swallow a capsule that has a camera in it. The images are transmitted to a recorder you wear on your belt, after which the capsule exits your body painlessly in your stool. You may still need an endoscopy with a biopsy to confirm a diagnosis of Crohn's disease. Capsule endoscopy should not be performed if a bowel obstruction is suspected.
Capsule endoscopy - This test is sometimes used to help diagnose Crohn's disease involving your small intestine. You swallow a capsule that has a camera in it. The images are transmitted to a recorder you wear on your belt, after which the capsule exits your body painlessly in your stool. You may still need an endoscopy with a biopsy to confirm a diagnosis of Crohn's disease. Capsule endoscopy should not be performed if a bowel obstruction is suspected.
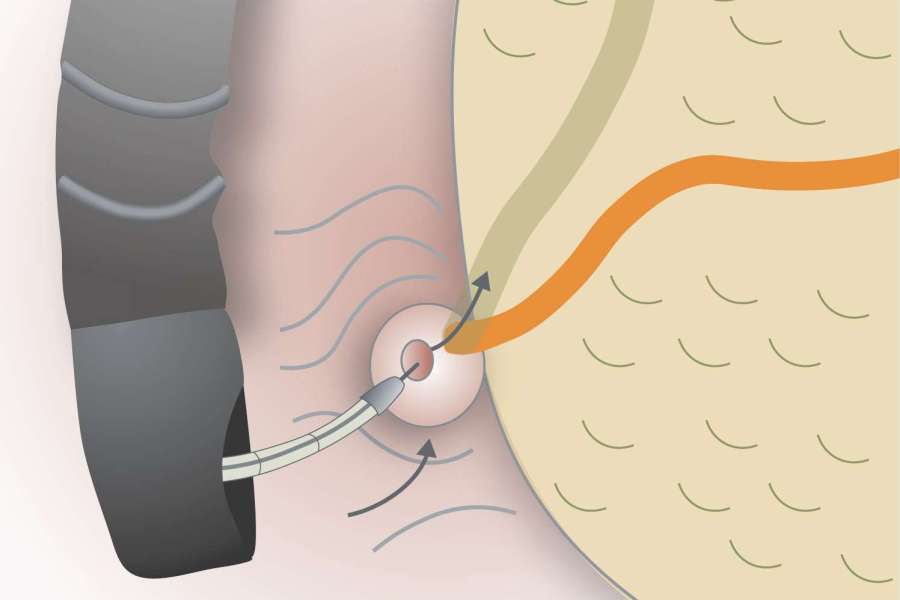
![]() Balloon-assisted enteroscopy - For this test, a scope is used in conjunction with a device called an overtube. This enables the technician to look further into the small bowel where standard endoscopes don't reach. This technique is useful when a capsule endoscopy shows abnormalities, but the diagnosis is still in question.
Balloon-assisted enteroscopy - For this test, a scope is used in conjunction with a device called an overtube. This enables the technician to look further into the small bowel where standard endoscopes don't reach. This technique is useful when a capsule endoscopy shows abnormalities, but the diagnosis is still in question.
![]() X-ray - If you have severe symptoms, your provider may use a standard X-ray of your abdominal area to rule out serious complications, such as megacolon or a perforated colon.
X-ray - If you have severe symptoms, your provider may use a standard X-ray of your abdominal area to rule out serious complications, such as megacolon or a perforated colon.
![]() Computerized tomography (CT) scan - You may have a CT scan — a special X-ray technique that provides more detail than a standard X-ray does. This test looks at the entire bowel as well as at tissues outside the bowel. CT enterography is a special CT scan that provides better images of the small bowel. This test has replaced barium X-rays in most medical centers.
Computerized tomography (CT) scan - You may have a CT scan — a special X-ray technique that provides more detail than a standard X-ray does. This test looks at the entire bowel as well as at tissues outside the bowel. CT enterography is a special CT scan that provides better images of the small bowel. This test has replaced barium X-rays in most medical centers.
![]() Magnetic resonance imaging (MRI) - An MRI scanner uses a magnetic field and radio waves to create detailed images of organs and tissues. An MRI is particularly useful for evaluating a fistula around the anal area (pelvic MRI) or the small intestine (MR enterography). Unlike CT, there is no radiation exposure with MRI.
Magnetic resonance imaging (MRI) - An MRI scanner uses a magnetic field and radio waves to create detailed images of organs and tissues. An MRI is particularly useful for evaluating a fistula around the anal area (pelvic MRI) or the small intestine (MR enterography). Unlike CT, there is no radiation exposure with MRI.

The goal of inflammatory bowel disease treatment is to reduce the inflammation that triggers your signs and symptoms. In the best cases, this may lead not only to symptom relief but also to long-term remission and reduced risks of complications. IBD treatment usually involves either drug therapy or surgery.
![]() Anti-inflammatory drugs - Anti-inflammatory drugs are often the first step in the treatment of ulcerative colitis, typically for mild to moderate disease. Anti-inflammatories include aminosalicylates, such as mesalamine (Delzicol, Rowasa, others), balsalazide (Colazal) and olsalazine (Dipentum).
Anti-inflammatory drugs - Anti-inflammatory drugs are often the first step in the treatment of ulcerative colitis, typically for mild to moderate disease. Anti-inflammatories include aminosalicylates, such as mesalamine (Delzicol, Rowasa, others), balsalazide (Colazal) and olsalazine (Dipentum).
![]() Time-limited courses of corticosteroids are also used to induce remission. In addition to being anti-inflammatory, steroids are immunosuppressing. Which medication you take depends on the area of your colon that's affected.
Time-limited courses of corticosteroids are also used to induce remission. In addition to being anti-inflammatory, steroids are immunosuppressing. Which medication you take depends on the area of your colon that's affected.
![]() Immune system suppressors - These drugs work in a variety of ways to suppress the immune response that releases inflammation-inducing chemicals into the body. When released, these chemicals can damage the lining of the digestive tract.
Immune system suppressors - These drugs work in a variety of ways to suppress the immune response that releases inflammation-inducing chemicals into the body. When released, these chemicals can damage the lining of the digestive tract.
![]() Biologics - Biologics are a newer category of therapy in which therapy is directed toward neutralizing proteins in the body that are causing inflammation. Some are administered via intravenous (IV) infusions and others are injections you give yourself. Examples include infliximab (Remicade), adalimumab (Humira), golimumab (Simponi), certolizumab (Cimzia), vedolizumab (Entyvio), ustekinumab (Stelara), and risankizumab (Skyrizi).
Biologics - Biologics are a newer category of therapy in which therapy is directed toward neutralizing proteins in the body that are causing inflammation. Some are administered via intravenous (IV) infusions and others are injections you give yourself. Examples include infliximab (Remicade), adalimumab (Humira), golimumab (Simponi), certolizumab (Cimzia), vedolizumab (Entyvio), ustekinumab (Stelara), and risankizumab (Skyrizi).
![]() Antibiotics may be used in addition to other medications or when infection is a concern — in cases of perianal Crohn's disease, for example. Frequently prescribed antibiotics include ciprofloxacin (Cipro) and metronidazole (Flagyl).
Antibiotics may be used in addition to other medications or when infection is a concern — in cases of perianal Crohn's disease, for example. Frequently prescribed antibiotics include ciprofloxacin (Cipro) and metronidazole (Flagyl).
![]() Other medications and supplements - In addition to controlling inflammation, some medications may help relieve your signs and symptoms, but always talk to your doctor before taking any over-the-counter medications. Depending on the severity of your IBD, your doctor may recommend one or more of the following:
Other medications and supplements - In addition to controlling inflammation, some medications may help relieve your signs and symptoms, but always talk to your doctor before taking any over-the-counter medications. Depending on the severity of your IBD, your doctor may recommend one or more of the following:
![]() Anti-diarrheal medications. A fiber supplement — such as psyllium powder (Metamucil) or methylcellulose (Citrucel) — can help relieve mild to moderate diarrhea by adding bulk to your stool. For more severe diarrhea, loperamide (Imodium A-D) may be effective.
Anti-diarrheal medications. A fiber supplement — such as psyllium powder (Metamucil) or methylcellulose (Citrucel) — can help relieve mild to moderate diarrhea by adding bulk to your stool. For more severe diarrhea, loperamide (Imodium A-D) may be effective.
![]() Pain relievers - For mild pain, your doctor may recommend acetaminophen (Tylenol, others). However, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diclofenac sodium likely will make your symptoms worse and can make your disease worse as well.
Pain relievers - For mild pain, your doctor may recommend acetaminophen (Tylenol, others). However, ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve) and diclofenac sodium likely will make your symptoms worse and can make your disease worse as well.
Vitamins and supplements. If you're not absorbing enough nutrients, your doctor may recommend vitamins and nutritional supplements.
![]() Nutritional support - When weight loss is severe, your doctor may recommend a special diet given via a feeding tube (enteral nutrition) or nutrients injected into a vein (parenteral nutrition) to treat your IBD. This can improve your overall nutrition and allow the bowel to rest. Bowel rest can reduce inflammation in the short term.
Nutritional support - When weight loss is severe, your doctor may recommend a special diet given via a feeding tube (enteral nutrition) or nutrients injected into a vein (parenteral nutrition) to treat your IBD. This can improve your overall nutrition and allow the bowel to rest. Bowel rest can reduce inflammation in the short term.
![]() Surgery - If diet and lifestyle changes, drug therapy, or other treatments don't relieve your IBD signs and symptoms, your provider may recommend surgery.
Surgery - If diet and lifestyle changes, drug therapy, or other treatments don't relieve your IBD signs and symptoms, your provider may recommend surgery.
![]() Surgery for ulcerative colitis. Surgery involves removal of the entire colon and rectum and the production of an internal pouch attached to the anus that allows bowel movements without a bag. In some cases a pouch is not possible. Instead, surgeons create a permanent opening in your abdomen (ileal stoma) through which stool is passed for collection in an attached bag.
Surgery for ulcerative colitis. Surgery involves removal of the entire colon and rectum and the production of an internal pouch attached to the anus that allows bowel movements without a bag. In some cases a pouch is not possible. Instead, surgeons create a permanent opening in your abdomen (ileal stoma) through which stool is passed for collection in an attached bag.
![]() Surgery for Crohn's disease. Up to two-thirds of people with Crohn's disease will require at least one surgery in their lifetime. However, surgery does not cure Crohn's disease.
Surgery for Crohn's disease. Up to two-thirds of people with Crohn's disease will require at least one surgery in their lifetime. However, surgery does not cure Crohn's disease.
During surgery, your surgeon removes a damaged portion of your digestive tract and then reconnects the healthy sections. Surgery may also be used to close fistulas and drain abscesses.
The benefits of surgery for Crohn's disease are usually temporary. The disease often recurs, frequently near the reconnected tissue. The best approach is to follow surgery with medication to minimize the risk of recurrence.

Our unhealthy lifestyle takes a heavy toll on the gastrointestinal health. Acidity and heart burn are the most oommon problems suffered by even young people.
These are lifestyle diseases and require lifestyle modification. The doctor needs to spend time and understand the unique problem of each patient to be able to suggest the right kind of lifestyle changes.
Dr. Mayank Chugh
Acidity & Gastric Diseases Specialist