GI bleeding can make the stool to look black. The level of bleeding can range from mild to severe and can be life-threatening.
If the stool looks black or dark brown then immediately consult a physician. Some blood tests and imaging tests can usually locate the source of the bleeding inside the gastro-intestinal system. Once the source of bleeding is established then treatment can be done.
Sometimes the bleeding can be seen (overt) and sometimes it can be hidden. This hidden bleeding is called Occult blood. The symptoms will also depend on the type of bleeding.
Overt bleeding might show up as:
![]() Dark brown blood in the vomiting
Dark brown blood in the vomiting
![]() Black or dark brown stool
Black or dark brown stool
![]() Blood coming out from the rectum
Blood coming out from the rectum
With occult bleeding, you might have:
![]() Lightheadedness
Lightheadedness
![]() Difficulty breathing
Difficulty breathing
![]() Fainting
Fainting
![]() Chest pain
Chest pain
![]() Abdominal pain
Abdominal pain

Your doctor will take history of past bleed and do a thorough physical examination before ordering the tests to diagnose the cause of GI Bleed. These tests may include :
![]() Blood tests - You may need a complete blood count, a test to see how fast your blood clots, a platelet count and liver function tests.
Blood tests - You may need a complete blood count, a test to see how fast your blood clots, a platelet count and liver function tests.
![]() Stool tests - Analyzing your stool can help determine the cause of occult bleeding.
Stool tests - Analyzing your stool can help determine the cause of occult bleeding.
![]() Nasogastric lavage. A tube is passed through your nose into your stomach to remove your stomach contents. This might help determine the source of your bleed.
Nasogastric lavage. A tube is passed through your nose into your stomach to remove your stomach contents. This might help determine the source of your bleed.
![]() Upper GI endoscopy - This procedure uses a tiny camera on the end of a long tube, which is passed through your mouth to enable your doctor to examine your upper gastrointestinal tract.
Upper GI endoscopy - This procedure uses a tiny camera on the end of a long tube, which is passed through your mouth to enable your doctor to examine your upper gastrointestinal tract.
![]() Colonoscopy - This procedure uses a tiny camera on the end of a long tube, which is passed through your rectum to enable your doctor to examine your large intestine and rectum.
Colonoscopy - This procedure uses a tiny camera on the end of a long tube, which is passed through your rectum to enable your doctor to examine your large intestine and rectum.
![]() Capsule endoscopy - In this procedure, you swallow a vitamin-size capsule with a tiny camera inside. The capsule travels through your digestive tract taking thousands of pictures that are sent to a recorder you wear on a belt around your waist. This enables your doctor to see inside your small intestine.
Capsule endoscopy - In this procedure, you swallow a vitamin-size capsule with a tiny camera inside. The capsule travels through your digestive tract taking thousands of pictures that are sent to a recorder you wear on a belt around your waist. This enables your doctor to see inside your small intestine.
![]() Flexible sigmoidoscopy - A tube with a light and camera is placed in your rectum to look at your rectum and the last part of the large intestine that leads to your rectum (sigmoid colon).
Flexible sigmoidoscopy - A tube with a light and camera is placed in your rectum to look at your rectum and the last part of the large intestine that leads to your rectum (sigmoid colon).
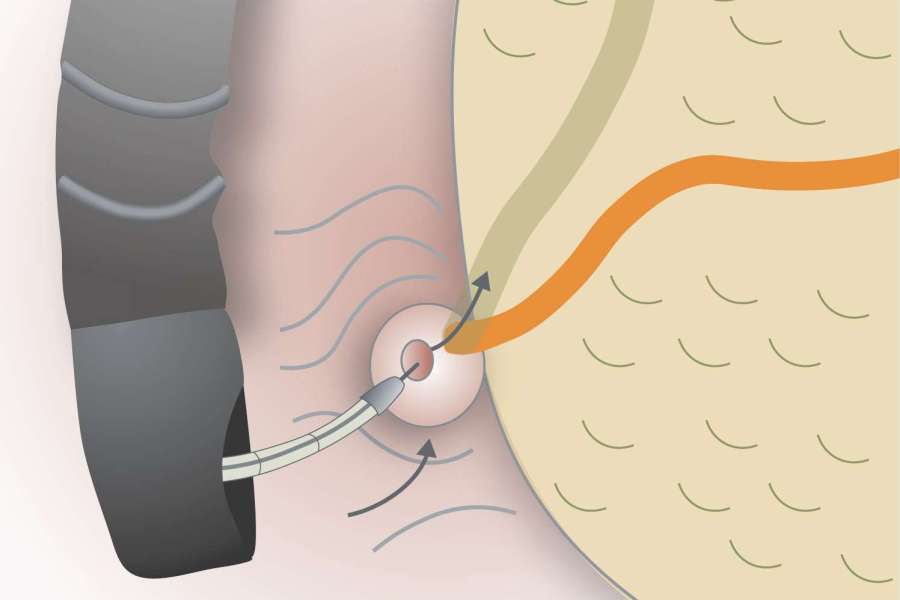
![]() Balloon-assisted enteroscopy - A specialized scope inspects parts of your small intestine that other tests using an endoscope can't reach. Sometimes, the source of bleeding can be controlled or treated during this test.
Balloon-assisted enteroscopy - A specialized scope inspects parts of your small intestine that other tests using an endoscope can't reach. Sometimes, the source of bleeding can be controlled or treated during this test.
![]() Angiography - A contrast dye is injected into an artery, and a series of X-rays are taken to look for and treat bleeding vessels or other abnormalities.
Angiography - A contrast dye is injected into an artery, and a series of X-rays are taken to look for and treat bleeding vessels or other abnormalities.
![]() Imaging tests - A variety of other imaging tests, such as an abdominal CT scan, might be used to find the source of the bleed.
Imaging tests - A variety of other imaging tests, such as an abdominal CT scan, might be used to find the source of the bleed.
There are several ways in which GI Bleed can be prevented from occuring. These include :
![]() Limit your use of nonsteroidal anti-inflammatory drugs.
Limit your use of nonsteroidal anti-inflammatory drugs.
![]() Limit your use of alcohol.
Limit your use of alcohol.
![]() Cut down on smoking.
Cut down on smoking.
![]() If you have GERD, follow your doctor's instructions for treating it.
If you have GERD, follow your doctor's instructions for treating it.
Often, GI bleeding stops on its own. If it doesn't, treatment depends on where the bleed is from. In many cases, medication or a procedure to control the bleeding can be given during some tests. For example, it's sometimes possible to treat a bleeding peptic ulcer during an upper endoscopy or to remove polyps during a colonoscopy.
If you have an upper GI bleed, you might be given an IV drug known as a proton pump inhibitor (PPI) to suppress stomach acid production. Once the source of the bleeding is identified, your doctor will determine whether you need to continue taking a PPI.
Depending on the amount of blood loss and whether you continue to bleed, you might require fluids through a needle (IV) and, possibly, blood transfusions. If you take blood-thinning medications, including aspirin or nonsteroidal anti-inflammatory medications, you might need to stop.

Our unhealthy lifestyle takes a heavy toll on the gastrointestinal health. Acidity and heart burn are the most oommon problems suffered by even young people.
These are lifestyle diseases and require lifestyle modification. The doctor needs to spend time and understand the unique problem of each patient to be able to suggest the right kind of lifestyle changes.
Dr. Mayank Chugh
Acidity & Gastric Diseases Specialist